Can Stem Cells Fix a Discogenic Back Pain?
Discogenic low back pain is a disabling condition. It is the third largest healthcare expense in the U.S. It is also second only to the common cold as a cause of missed work.
Many people who live with discogenic back pain have limited treatment options. Non-surgical treatments, such as physical therapy and opioid pain medication, aren’t always effective.
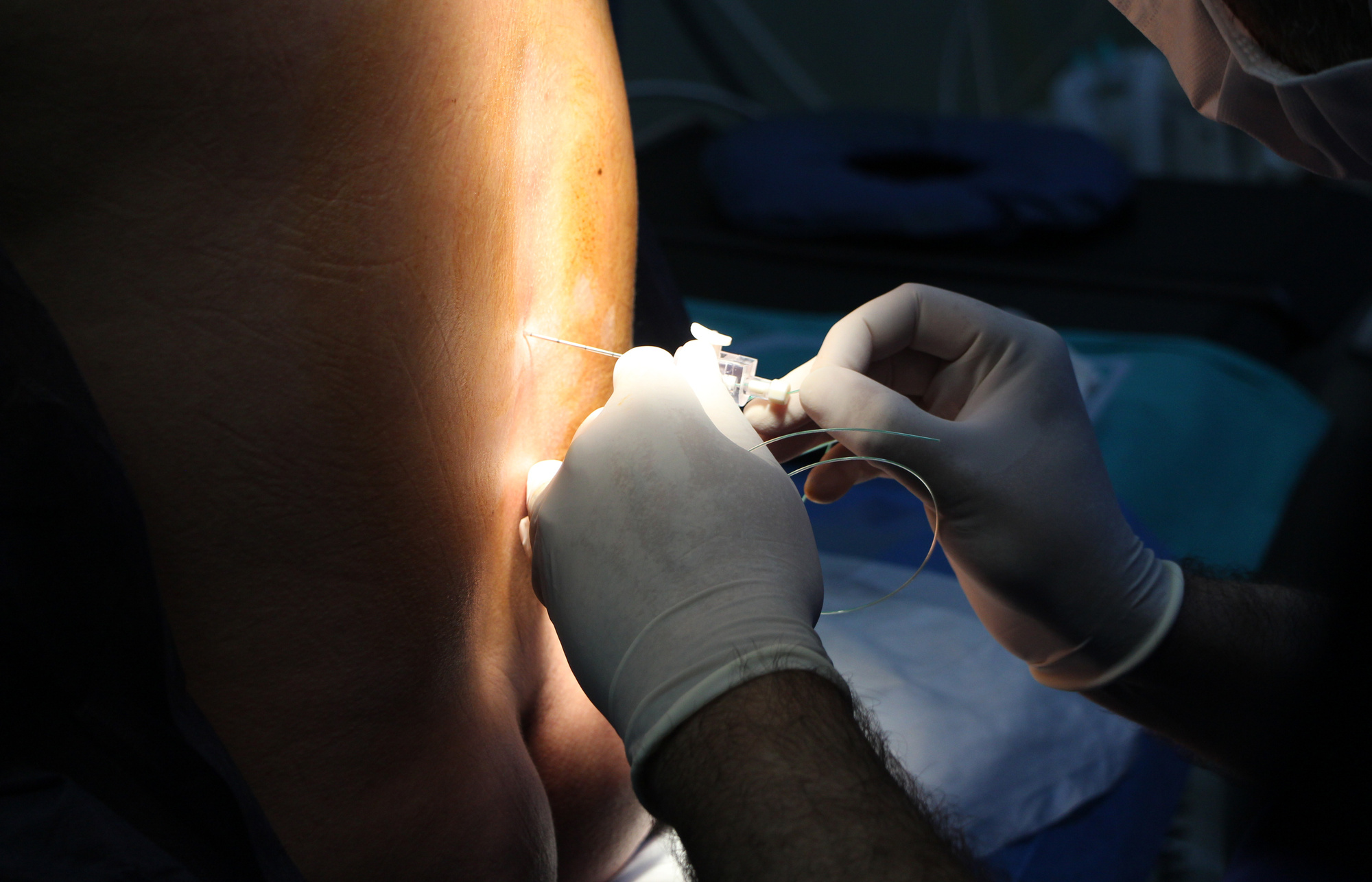
The injection of stem cells into the disc is being pursued as an alternative to both non-surgical and surgical treatments.
Read further to learn more about this exciting, new technique that offers long-term pain relief.
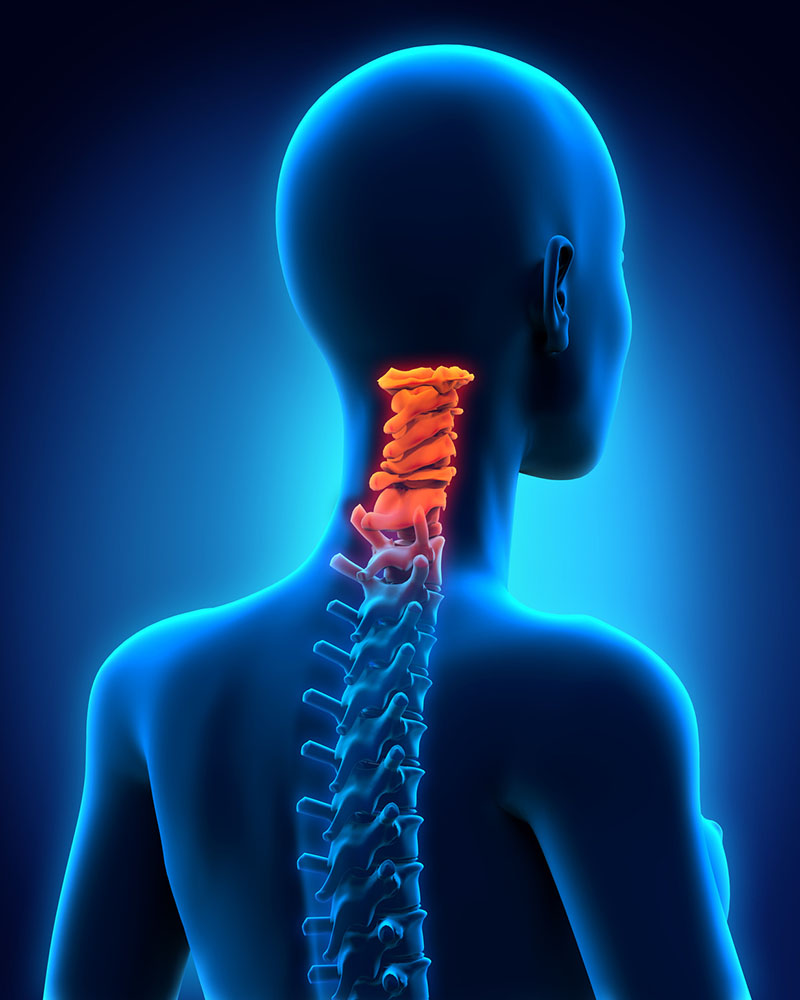
Discogenic Back Pain
Discogenic pain begins from one or more damaged spinal discs. It is usually due to degenerative disc disease and happens naturally with age. Sometimes, a ruptured or herniated disc is the cause of pain. It is rarely seen after 60 years of age.
Symptoms of this disorder include:
- Increased pain when sitting, coughing and sneezing, and leaning forward
- Leg pain, called radiculopathy, when sitting, standing, and walking
- Usually chronic in nature
Discogenic pain is most often diagnosed by MRI. When standard treatments fail, the physician orders a discography (or discogram). This is a special x-ray where the radiologist injects dye into the discs and takes x-rays. It helps determine if the patient has more than one disc causing the pain.
The most common treatment for this disorder is surgery, which has many risks. Other treatments include physical therapy, medications, and spinal injections. Alternative therapies such as acupuncture and yoga may also be helpful.
Doctors are now turning to stem cell therapy to treat patients with uncontrolled back pain.
Stem Cells and Pain Management
Stem cells are cells that have not transformed into their specific function in the body. They include bone marrow, skin cells, and embryonic cells. Their main function is to replace damaged cells and promote tissue regeneration.
The doctor aspirates bone marrow from the hip bone of the patient. The bone marrow has many different types of cells including stem cells. Then, the lab spins the aspirated sample in a centrifuge to separate the different types of cells.
Stem cell disc regeneration is the process where the physician injects the cells into a patient’s spine. He/she uses x-ray imaging as guidance to locate the correct location. With time, the cells begin to differentiate with the growth of new disc tissue. Complete disc regeneration occurs from a couple months to a year. Many patients experience total relief of their pain within a few months.
Researchers reviewed many studies using different types of stem cells. They found improvement in discogenic pain in all but one study.
Researchers think stem cells work to decrease the pain and inflammation in the spine. They also function to repair the damaged tissue. These studies show that stem cells can increase the new growth of the disc tissue.
The exact mechanisms of this novel treatment are still unknown. Yet, it creates a less invasive choice for people suffering from back pain.
Patient Criteria
Because this is such a new therapy, there are no official guidelines in place. Some physicians recommend it for younger patients with mild disc damage. Others make the decision on a case-by-case basis. The patient also needs to know that health insurance doesn’t cover it. Most facilities require cash payments.
Risks and Benefits
Stem cell therapy is so new that the long-term risks and benefits are still unknown.
Benefits include:
- Reduction of pain
- Decreased inflammation
- Replace bone, cartilage, and disc cells
- Less invasive and shorter recovery time than surgery
- Minimal pain with the procedure
- Little to no adverse effects
Risks involved include:
- The best stem cell type and the best way to administer it is unknown
- The potential for infection at aspiration and injection sites
- Pain and swelling
- Rash and redness at the site
There are no serious adverse effects reported to date. But, there are also no long-term studies to compare results. Doctors suggest weighing the pros and cons to determine if this is a good fit for each patient.
Questions for Your Doctor
Write down your questions before coming to the appointment. You won’t forget to ask about important concerns. You will leave informed and confident about your decision.
- How do you calculate the number of cells needed per injection?
- Is there a difference between stem cell therapy for disc regeneration and cancer therapy?
- What is the risk of contamination?
- Do other conditions like diabetes or smoking affect the regeneration?
- What is your success/fail rate?
- Have you seen any adverse side effects from this treatment?
Future Implications
There are still unknown aspects of stem cell therapy. Future research should include long-term studies to rule out complications not already known.
In the future, the use of stem cells can decrease or end the pain. It can help avoid thousands of unnecessary surgeries. The disc causes unbearable back pain when they deteriorate. There is no cushion from the discs creating unrelenting pain.
Researchers expect to slow down the breakdown of aging discs. Initial data from current research shows this is a promising therapy for discogenic back pain.
How We Can Help
Stem cell therapy often gives welcomed relief from this painful condition. It also creates the regeneration of tissue to heal the damaged discs. Patients who have exhausted all available treatments now have an alternative to surgery.
There are no guarantees with any medical procedure. Alternatives for these patients include surgery and narcotic pain medications.
Understanding the use of stem cell therapies is crucial for patients to weigh all their options. Sometimes this is the only treatment option left. It provides a better solution while decreasing the time for recovery and the costs seen with surgery.
Disk regeneration helps patients suffering from long-term, disabling pain. It allows them to return to a life without pain. They can begin to take part in activities that their pain prevented them from doing.
If you’re dealing with disabling back pain, contact us to find out if stem cell therapy is for you. We will direct you to the next steps to take to find out if you are a good candidate for the procedure.