Can Scoliosis be Cured?
The transition between our early childhood and teenage years is a complicated weave of emotions, hormones, and life transitions. Yet that period can be far more stressful when combined with scoliosis.
A condition most often diagnosed during the puberty stage of one’s life, scoliosis can range from mild to severe. Left untreated, it can impact your posture and even endanger your health.
But what is it, exactly?
More importantly, can scoliosis be cured?
What is Scoliosis?
Scoliosis is a condition where the spine curves as it grows. It affects both the neurological and the muscular systems. This curve can either form in a “C” shape or back and forth like an “S”.
There are four different types of scoliosis:
- Idiopathic Scoliosis, which has no known origin
- Neuromuscular Scoliosis, which is caused by neuromuscular disorders
- Congenital Scoliosis, which is a rare genetic defect
- Degenerative Scoliosis, which develops in older adults
Most patients start to see symptoms of this abnormality between the ages of 10 and 14. This is because your body is growing and developing. Typically, you’ll see the most impact of your scoliosis during these formative years, but it can progress even after your teens.
This condition can occur in both male and female patients. However, it is more common amidst women.
What are the Symptoms of Scoliosis?
There are various signs of scoliosis. Some of them you can feel, while others you can see with the naked eye or on a medical scan. The most common include:
Seemingly Ill-fitting Clothes
Sometimes the symptom is as subtle as looking in the mirror and noticing your clothes don’t fit right.
You squint at your reflection, wondering why your shirt looks tighter in some areas than others, or why the edge of your shirt looks uneven compared to the opposite side.
This is caused by the tilt of your frame due to your spine’s curvature.
An Asymmetrical Back
Perhaps you are wearing a tank top or bathing suit when you, a friend, or family member notices your shoulders or back appear asymmetrical. This is another indicator of scoliosis.
A Change in Gait
Have you noticed yourself having trouble walking? Maybe your legs can’t seem to find the proper rhythm or one feels longer than the other. Scoliosis’ impact on your spin can misalign your hips, causing you to walk differently than normal.
You may even find yourself growing more fatigued since your body has to work harder to maintain balance.
A Noticeable Decrease in Range of Motion
As the spine begins to curve, it reduces its flexibility. Patients find it harder to bend their torso front to back or side to side.
An Increase in Back Pain
In severe cases of scoliosis, the curvature can lead to painful muscle spasms in the back, as well as deterioration of various discs and joints due to the strain.
Dangerous Levels of Pressure on Internal Organs
Scoliosis doesn’t just impact your skeletal frame. The sharp twists and angles can also cause pressure on your lungs and heart, hampering their function and creating hazardous health problems.
What are the Causes of Scoliosis?
While some cases of scoliosis may be caused by neuromuscular conditions like genetic defects, muscular dystrophy, or cerebral palsy, most cases have no defined cause.
Doctors have identified age, genetics, and sex as factors that play a role in how high a patient’s risk factor is in developing scoliosis. While most scoliosis patients have no prior history of it in their family, those whose family members have developed this condition are at a higher risk of doing so themselves.
Most cases develop during puberty, so young adults are less likely to receive scoliosis as a diagnosis. However, elderly adults may develop degenerative scoliosis after the age of 65.
Women are more likely to have this condition than men, but why it occurs still remains a mystery in most cases.
Can Scoliosis Be Cured?
While there is no cure for scoliosis, there are multiple scoliosis treatment options available on a case-by-case basis. First, a doctor must diagnose a patient’s scoliosis as well as his or her degree of severity.
This is done through imaging tests in order to identify the shape of your spine, as well as any underlying causes, such as an injury or the growth of a tumor.
For mild cases, your doctor may simply suggest monitoring your scoliosis, especially during your teen years. Since your body grows so rapidly during this period, your scoliosis also evolves rapidly.
If this is the case for you, your doctor will expect to schedule an appointment about once every six months.
Left unattended, scoliosis can damage the heart and lungs, cause severe back problems, and misalign your skeleton. If the scoliosis is severe then your doctor may require medical intervention.
This could include a brace or even surgery to help slow or reduce your spine’s curve. A brace is typically worn during a patient’s pubescent period in order to guide the spine into better alignment as it grows. This brace isn’t required after your bones have finished their growth period.
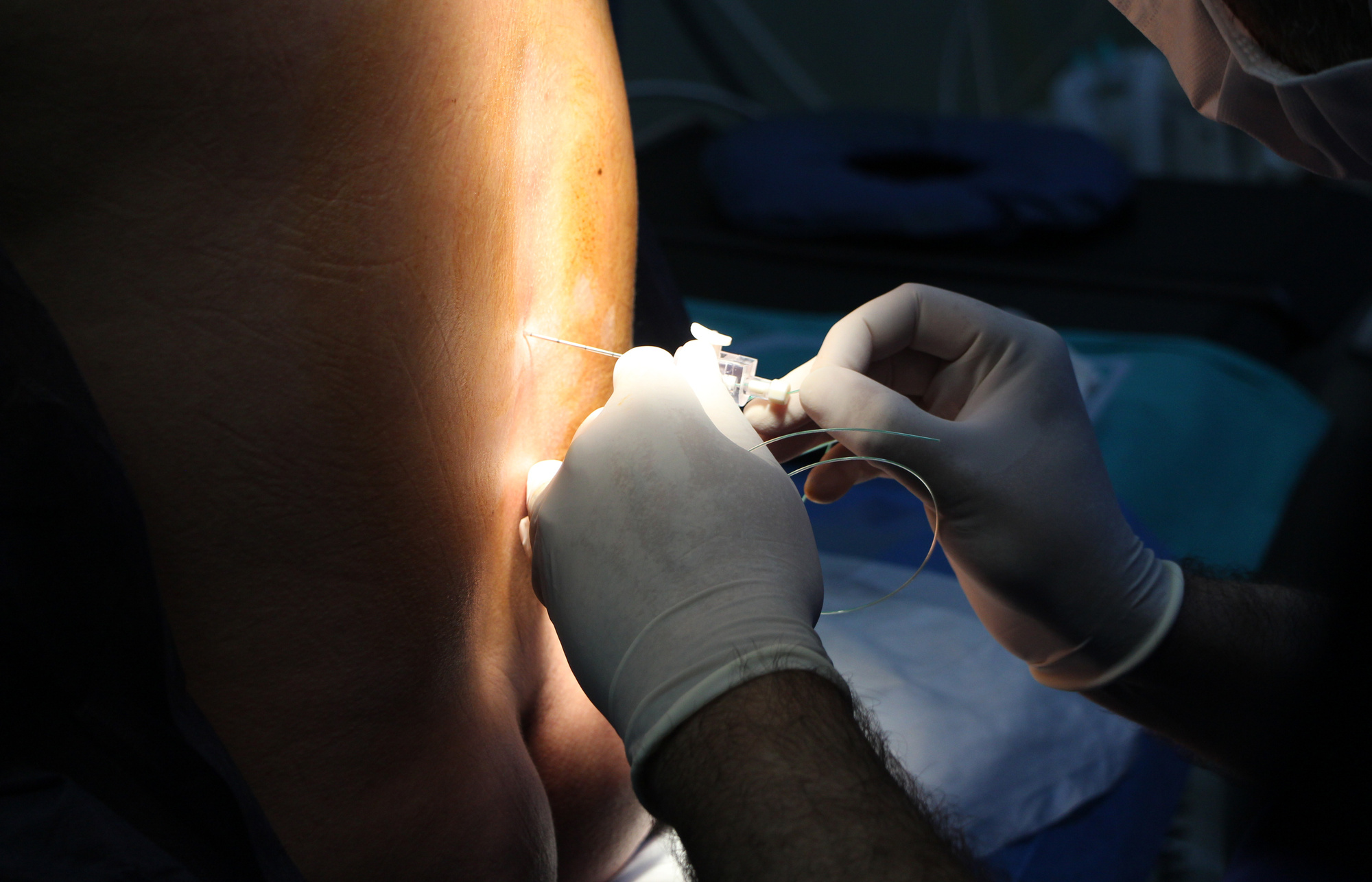
If surgery is required, this is typically done through a spinal fusion or installation of a metal rod. Although similar, these two forms of surgery implement a different approach to spinal realignment.
Spinal fusion uses small rods, wires, or other metal pieces to fuse certain vertebrae together. While this stiffens the back, it can improve the overall alignment.
The rod installation is a larger piece of hardware that is adjusted as the patient grows. Like the check-up appointments, these adjustments are made approximately once every six months.
Do You Think You Might Have Scoliosis?
While the answer to “Can scoliosis be cured?” may not be the one you were looking for, the good news is that there are many treatment options. If caught early enough, most patients can go on to lead normal, healthy, happy lives.
If you or a loved one are experiencing symptoms of scoliosis, contact your doctor. Patients in Hackettstown and Newton, New Jersey can book an appointment with our spinal surgery office without ever leaving their computer chair.