Finding the Source: 7 of the Most Common Causes of Back Pain
How long have you had your mattress? Be honest…
If you can’t remember the last time you got a new mattress, it’s time to hit the furniture store.
Why? Because sleeping on an old mattress is killer on your back.
But a bad mattress isn’t the only thing that can put your back in a bad mood. Lots of other lifestyle factors and medical issues cause back pain. And it’s important to know those causes so you can do your best to prevent back injuries in the future.
In this article, we’ll take a closer look at 7 of the most common back pain causes and what you can do to prevent them.
Common Back Pain Causes
There are certain risk factors that make you more susceptible to back problems. People who are overweight are more at risk. And if you’re not moving around much, you’re more likely to injure your back.
If you work in a job that requires heavy lifting or long periods of standing on your feet, you’re more likely to have spine pain. And as you age, you might develop back pain because of wear and tear on your muscles and spine.
Knowing your risk factors can help you prevent back injuries. But no matter how much you work to prevent them, there’s still a chance you’ll experience problems at some point during your life. Now let’s look at the 7 most common causes of back injuries.
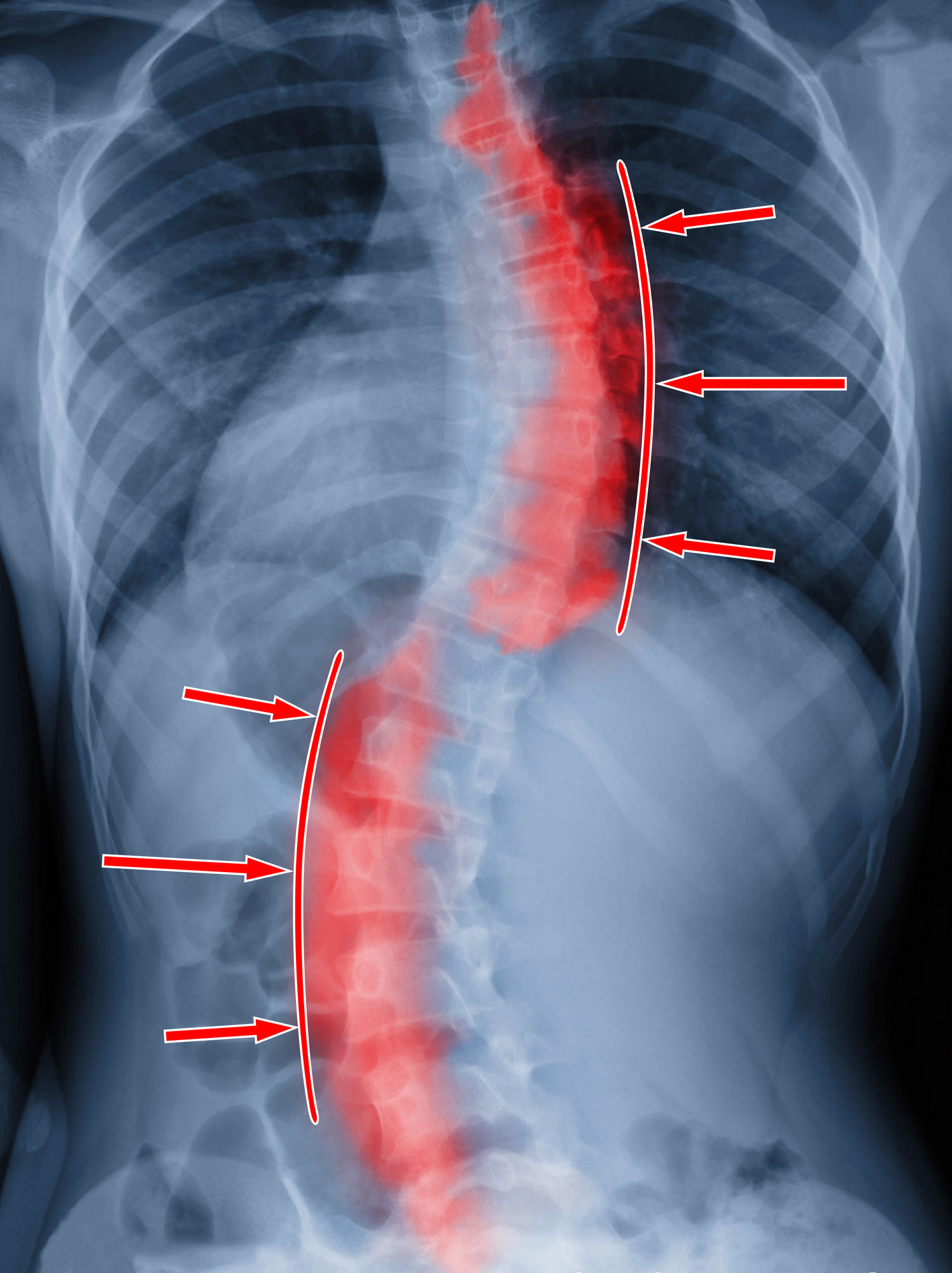
1. Slouching
The way you hold up your body affects back health. Working long hours at a desk without taking a break can cause you back pain. And if you do this over a lifetime, it can compound into more serious issues like herniated discs and arthritis.
Also, bending your neck forward too much can make your back to hurt. This is a problem called text neck. And it’s a serious issue affecting many smartphone users today.
To prevent this, pay special attention to your posture. Take breaks from sitting and walk around. And put your smartphone away before your neck gets tired.
2. Overuse
Sometimes, your back hurts because of a good, old-fashioned muscle injury. Muscle pulls and strains come about most often because of overuse.
It’s more likely to happen when you do exercises that you aren’t used to. Like when you haven’t played basketball in 10 years and you decide to join a game at the gym. The bending, reaching, and twisting can cause you to injure yourself.
But even seasoned athletes can overdo it and strain the muscles in their backs. Be aware of how your back feels while you’re exercising. Stop at the first sign of back pain to prevent further injury.
3. A Bad Mattress
We already mentioned this briefly, but let’s dive into your bedroom routine. You should replace your mattress at least every 10 years. But this isn’t a hard and fast rule.
Every person sleeps differently on their mattress. And every mattress wears differently. If you’re already having back problems, consider getting a new mattress sooner rather than later.
And consider upgrading your pillows too. Pillows bear the responsibility of holding up your head and keeping your neck in alignment. Old, flat pillows are just as likely to cause back problems as your mattress.
4. Arthritis
The most common form of arthritis is osteoarthritis. And lumbar arthritis happens when you develop osteoarthritis in your back. Over time, the cartilage in the joints wears down.
Without that cartilage, you lose range of motion, making the movement more painful. And it puts more stress on your nerves.
Prevent arthritis by maintaining a healthy weight and exercising. Also, eat a diet rich in foods that fight back pain.
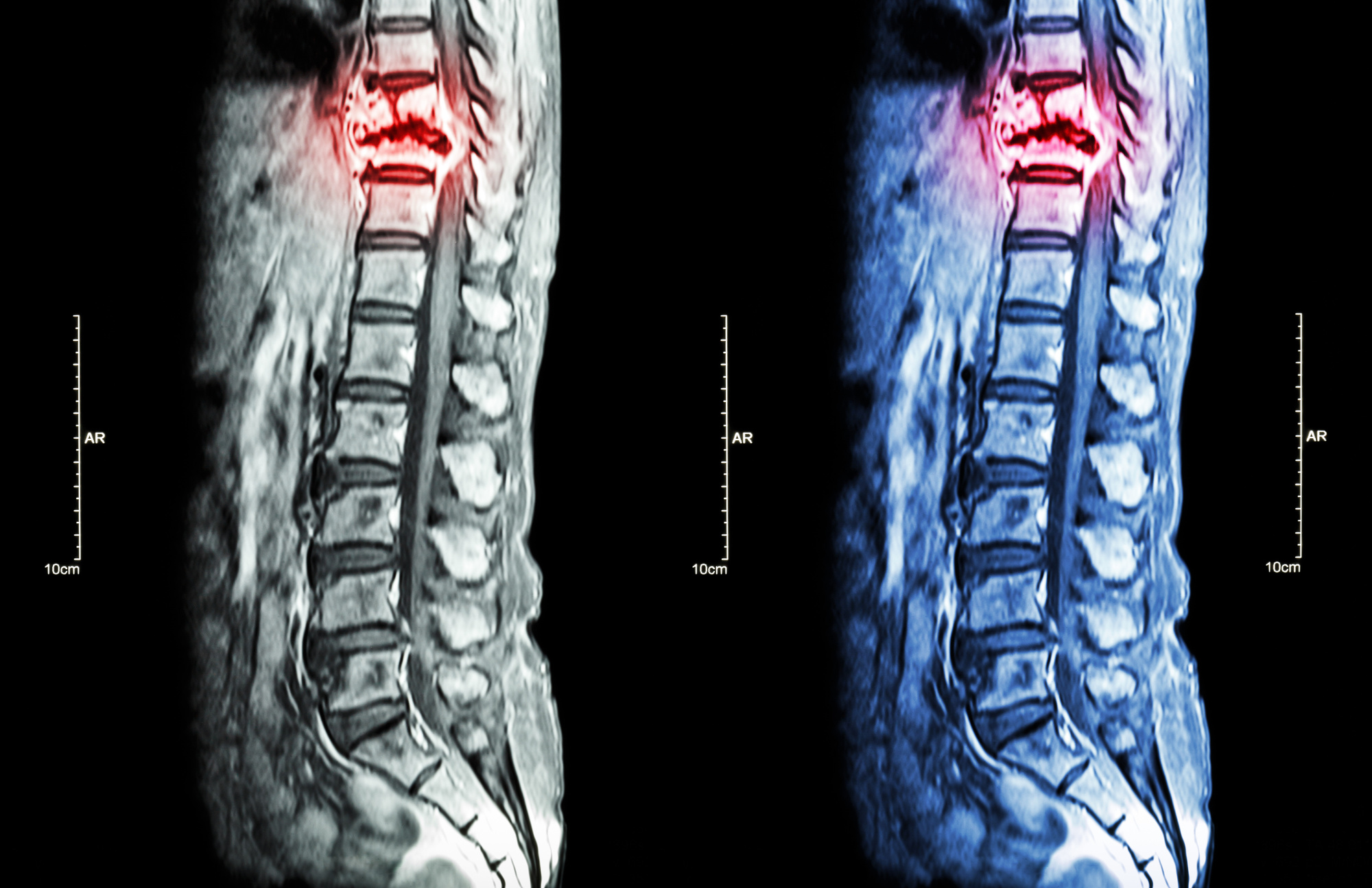
5. Osteoporosis
Osteoporosis develops when our bones lose minerals and weaken over time. The pain isn’t caused by the disease itself. It’s caused by tiny fractures in the bones of the spine that happen because the bones are so weak.
These fractures occur suddenly. You’ll notice a new pain in your spine because of a certain movement, even from a cough or sneeze.
Unfortunately, many people (women especially) are prone to developing osteoporosis. But preventative measures like eating foods rich in calcium and vitamin D are helpful. And weight-bearing exercises strengthen bones and prevent or prolong osteoporosis development.
6. Disc Problems
Each vertebra is separated from its neighbors by spongy discs. These discs are little fluid-filled sacs that provide a cushion for the bones around them. As you age, or if you suffer a spinal injury, these discs can get injured too.
A bulging disc happens when the disc slips out of place and sticks out further on one side of the spine. This puts pressure on the nerves around the disc.
A ruptured disc occurs when aging or trauma causes the tear, releasing the fluid inside. This means the disc won’t provide as much cushion to the bones as it should. And that also means more pressure on the nerves in the area.
Prevent disc problems by regularly stretching your back. Also, using proper lifting techniques helps. And, of course, regular exercise keeps the back strong enough to shield the discs from injury.
7. Sciatica
Your sciatic nerve is the longest nerve in your body. It runs from the lower back down through your hips and thighs, all the way to your feet. Sciatica is when that nerve becomes pinched or inflamed.
This is usually caused by a bulging disc as we mentioned before. But it can also come from bone spurs or hip and back injuries.
Sciatica pain starts in the lower back and can spread down into the legs and feet. It may be sharp or dull, depending on how much pressure is on the nerve.
Prevent sciatica by doing the same things you’d do to prevent a bulging or ruptured disc, as these are the most common causes of sciatica.
Treat Back Pain ASAP
Many people experience back pain at some point in their lives. These back pain causes are some of the most common. You can prevent these issues by maintaining a healthy weight, keeping good posture, and exercising.
But remember, it’s not normal to have back pain. If you do suffer from back problems, get it looked at asap. It might be a sign of something worse.
At Executive Spine Surgery, we take a multidisciplinary approach to give you the best possible treatment for back pain. Visit our website to book your appointment online to see Dr. Spivak.
Don’t live with back pain anymore. Get it treated now!