How Does Stem Cell Disc Regeneration Work?
For many people, pain in the legs, hip, and back can be quite unpleasant.
One common cause of this pain is a degenerated disc, which is also known as degenerative disc disease. In the US, this condition is common as there are about 3 million cases every year.
Well, there are different treatments for such pain, including physical therapy, muscle relaxants, analgesic, nucleoplasty, and nonsteroidal non-inflammatory drugs. Surgical procedures may also be necessary for some instances.
One of the recent additions to the treatment options is stem cell disc regeneration. This procedure is already being advertised as an effective option for back pain. But, do you know how it works?
Keep on reading to learn more.
What Is Degenerative Disc Disease?
Degenerative disc disease occurs when normal activities that occur in the disc cause pain.
Ideally, these activities take place in nearly everyone over time. However, not everyone feels pain. Depending on your lifestyle, the disc can wear faster than in other people. When they get worn-out, you’ll start feeling pain.
Discs in the spine are made up of water. As you age, the water is lost, and the discs become thinner than before. This means your discs can’t absorb shock well. Also, they’re less cushioned, and this increases your risk of low back pain.
Also, the stress of daily activities can lead to tiny tears in the out water that contains nerves. Your discs may push through the tears, and this is what’s known as a herniated disc. When this happens, you’ll feel pain.
What is Stem Cell Disc Regeneration?
This is typically a medical process that involves the injection of stem cells into the disc. According to its proponents, the treatment works by preventing or slowing the degenerative process of the discs. It achieves this facilitating the production of new disc cells.
Scientists have already tried this injection on animals, such as rabbits, and it yielded promising results. As such, this has been a welcoming idea in the treatment of back pain in humans.
It’s hypothesized that stem cells turn into cartilage cells when injected into the disc. This allows the disc to regenerate and consequently, alleviating the pain. Doctors can harvest the stem cells from adults to use in treatment.
What Happens During the Procedure?
Well, the stem cell disc regeneration treatment is still in its infancy stage. However, experimental stem cell treatments have healed the damage that has occurred on the disc.
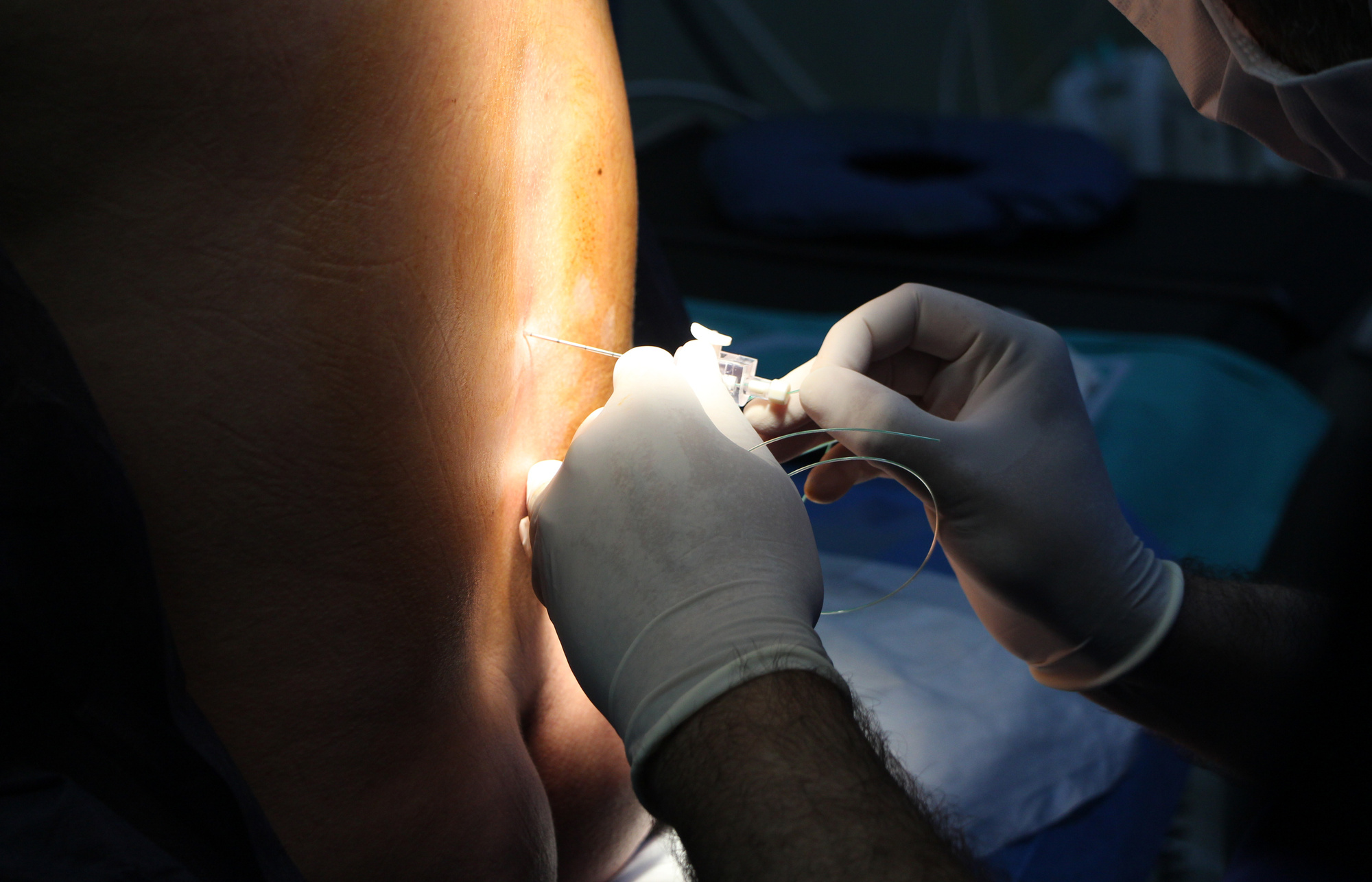
The procedure is minimally invasive. The doctor first extracts bone marrow from the patient’s hip bone. Then, they separate the stem cells through a procedure known as centrifugation. Alternatively, stem cells can be obtained from abdominal fat through a process called liposuction.
Your doctor will then use an X-ray to determine the ideal spot for injecting the stem cells. You can return to your normal routine after the injection.
Does it Work?
According to doctors, patients usually experience improvement two to three months after the treatment. Plus, you only need one treatment to get better.
However, in some cases, patients may need two or three injections. Also, a patient can’t have more than three injections within a span of 12 months.
Many doctors are claiming that disk regeneration using stem cells is the only effective alternative treatment for fusion and back surgery. It’s noted that the injection helps the disc to regenerate at a healthy rate. As such, patients should not worry about any possible complications.
Doctors also recommend undergoing physical rehabilitation following the treatment. Keep in mind that your recovery will depend on the degree of your spinal disc damage.
Why Use Stem Cells
Stem cells are ideal for this procedure because of their ability to repopulate. Essentially, they’re able to differentiate into discogenic cells.
In the past, doctors used to use embryonic stem cells. These are stem cells that are derived from the inner mass of the human embryo. Today, this is not the case since the adult stem cells are ideal for use, too.
Doctors can derive adult stem cells from the bone marrow or the adipose tissue. It’s noted that adipose-derived stem cells offer the ideal matrix for stem cell disc regeneration. This is because of their ability to generate the cartilage faster than bone marrow-derived cells.
Stem cells have also shown to communicate with nucleus pulpusus (NP) cells. This helps to produce anabolic growth factors that boost the cell function.
Possible Risks
As with any injection, there are potential risks, such as bleeding, infection, and nerve damage. Also, the risks depend on the area that’s receiving the injection.
It’s important to note that there’s no risk of allergy. This is because the doctor uses the patient’s own stem cells. With that in mind, every case is unique. At this time, there are no reports of any complications from patients.
There are FDA studies and trials that ongoing to help doctors understand more about the stem cell disc regeneration therapy.
What Does this Mean for Patients?
Several health centers and facilities, including Executive Spine Surgery, are already offering stem cell injections for degenerative discs. If you’re considering this treatment, it helps to find reputable doctors to provide it.
A good doctor will monitor your closely for potential benefits and side effects after getting the injection. Plus, they’ll help you know whether the treatment will work for you. This is because a severely degenerated disc has proven nearly irresponsive to treatment.
Severely degenerated discs that have lost all of their height usually have fewer cells living in them.
Final Thoughts
While stem cell disc regeneration has yielded promising results, it’s worth working with a doctor that assesses your situation well. Ideally, this treatment has considerable potential in revolutionizing the treatment of disc degeneration, herniations, and cartilage defects.
At Executive Spine Surgery, we treatment disc problems, such as bulbing, herniations, and degeneration. We offer a personalized approach to ensure all unique issues are addressed. THrough our minimally invasive treatments and pain management procedures, we’re sure to help you recover from your back pain.
Well, do you have any question about disc regeneration or back pain? Feel free to reach out to us, and we’ll be glad to help.