What Is the Role of PRP in Sacroiliitis?
Are you struggling with lower back pain? Do you deal with constant sciatic nerve pain? Does climbing stairs make your back hurt?
You’re not alone. You might be among the 40% of Americans who will suffer from this pain at some point in their lives.
Luckily, there’s a solution. It comes in the form of PRP, or Platelet Rich Plasma, injections.
Keep reading to find out everything you need to know about Sacroiliitis and PRP.
What Is Sacroiliitis?
First of all, let’s define Sacroiliitis. Sacroiliitis is the inflammation of both or one of the sacroiliac joints. These joints are situated in the spot where your pelvis connects to your lower spine– your lower back.
These joints are vertical and about 6 or 7 inches long. They’re held together by ligaments that contain tons of nerve receptors.
Since the sacrum is often subject to lots of stress as you go through your daily motions, the sacroiliac joints can become inflamed. This is what leads to Sacroiliitis. The many nerve receptors in the surrounding ligaments are responsible for the pangs of back pain that you may feel.
Sacroiliitis can cause pain in your back, buttocks, and can even extend all the way down your legs. It can also be hard to diagnose. Back pain is finicky, and the pain symptom is really the only telling symptom for sacroiliitis diagnosis.
Oftentimes, patients will come back with normal EMG studies, MRI scans, and lumbar spine scans. Yet they’ll still experience pain. Your doctor needs to be looking for Sacroiliitis to find it.
This is why it often takes time to diagnose. Usually, it’s a last resort diagnosis, after other scans have come back normal.
If your lower back pain gets worse when you climb stairs, stand for a prolonged period of time, or go for a run, you may have Sacroiliitis.
How Is It Caused?
There are five potential causes of sacroiliitis.
Traumatic injury is the first. This includes injuring your sacroiliac joints while lifting heavy items. It also includes injury from falling or getting into a car or bike accident.
A biomechanical injury is the second. This includes sacroiliac joint dysfunction manifesting from a previous lumbar infusion, or a discrepancy in leg length.
Hormonal imbalances or changes are the third. This includes hormonal changes due to medication, or natural hormonal changes due to pregnancy or childbirth.
Inflammation is the fourth. This is when your tissues become swollen, red, and painful.
The fifth is normal age-related degeneration, usually brought on by normal wear and tear over the years.
How Is It Diagnosed?
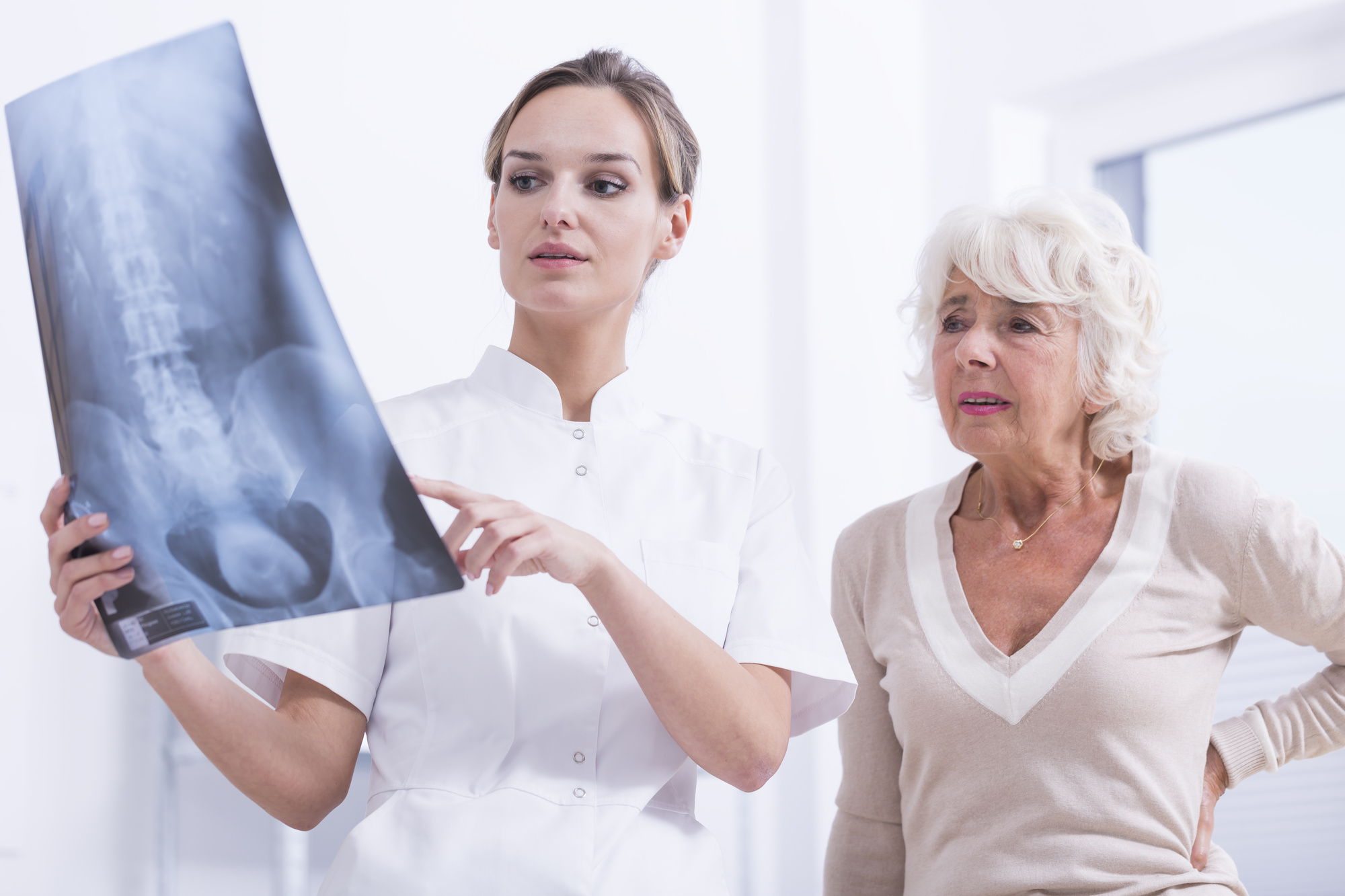
To diagnose sacroiliitis, you’ll need to first schedule doctor’s appointment. They’ll probably press on points of your lower back, including your buttocks, to try to put a finger on the location of the pain. Your doctor may order x-rays or an MRI of your back and sacroiliac joints to show if your sacroiliac joint is injured and to make sure the low back is not the cause of the pain. Another method your doctor will confirm the diagnose Sacroiliitis is anesthetic injections. This involves your doctor injecting the affected area with a numbing injection. If the pain stops, it’s likely that your sacroiliac joint is the problem.
The one caveat with this method of diagnosis is The anesthetic injection can leak into a surrounding area, making it unclear whether or not your sacroiliac joint is really the problem.
What Can You Do?
Physical therapy is an option. It’ll include plenty of strengthening and stretching exercises. If physical therapy doesn’t alleviate your symptoms, you might be a candidate for PRP, or Platelet Rich Plasma, injections.
How Does It Work?
Spinal injections are an effective pain management tool. PRP injections work to aid your boby in its natural healing process.
Platelets begin repairing your tissue by releasing growth factors. Growth factors are a substance, such as a hormone or a vitamin, that’s necessary to stimulate the growth of living cells.
The growth factors initiate the process of healing by attracting reparative cells, especially critical stem cells. Without PRP injections, your body would have far fewer platelets, meaning a slower healing time.
Once the platelets have been injected into your bloodstream, a sample of your blood will be taken and put into a centrifuge. The centrifuge will then separate the added platelets from the rest of your blood. Then, that concentration of PRP is re-injected into your body, specifically into your lower back.
Now, your lower back has tons of tools to begin healing– all naturally. After the injection, it takes around six weeks for your body to reduce inflammation and rebuild tissue within your sacroiliac joints. After six weeks, you’ll feel good as new.
When PRP Injections Aren’t Enough
You might get the PRP injections and find that your Sacroiliitis is just too far gone. While PRP injections are certainly effective for pain management, they can’t reverse degeneration or injury.
If this sounds like you, you might be a candidate for spinal surgery. If so, you should opt for a minimally invasive one.
Why? Because traditional surgery requires a very large incision. That means extensive tissue damage, and a subsequent long time recovering.
Why go the traditional route when a minimally invasive option is available?
Today, the minimally invasive procedure is as simple as placing three titanium implants on your sacroiliac joint. These implants will fuse and therefore stabilize the connection between the joints, your spine, and your pelvis.
It only takes around an hour, and you might even be discharged to go home the same day. That’s far preferable to weeks recovering in the hospital.
Are You a Candidate?
If you’re experiencing lower back pain, you could be struggling with Sacroiliitis and not know it yet. Oftentimes, sciatic nerve pain can go untreated for too long, and improperly diagnosed once you find the time to visit the doctor.
Don’t let this be you. If you’re in Hackettstown, Cedar Knolls, or Whiting, New Jersey, get in touch. We would love to get you on the road to recovery.