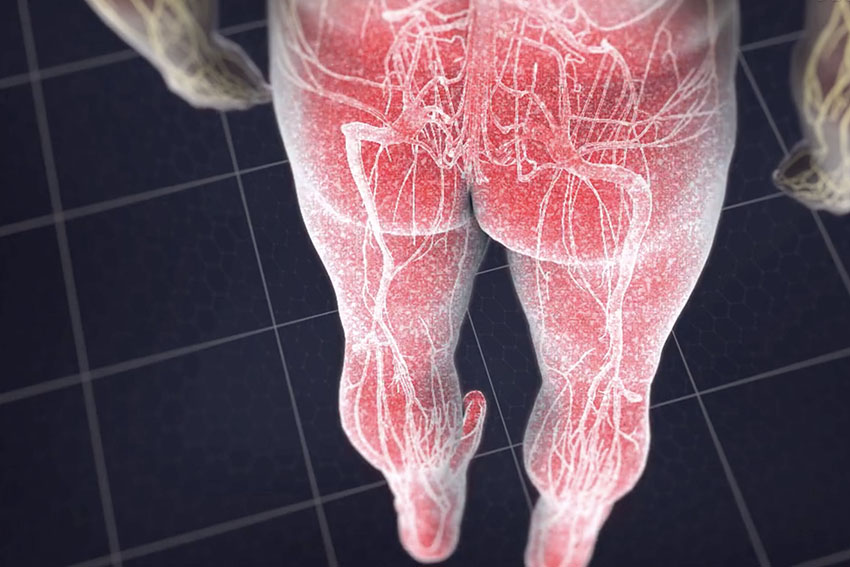
What is Sciatica?
As people age the spine slowly wears out through a process called degeneration. Degeneration is usually first seen in the disks in adults in their thirties to fifties. The annulus may weaken allowing the nucleus to bulge forming bulging disk. If the annulus tears, the nucleus may squeeze out forming a herniated disk. The disk may compress or “pinch” spinal nerves causing back and leg pain, numbness, tingling and weakness called sciatica. This pain may be worsened or maintained by inflammation around the nerve roots. Sciatica is a common problem that we see at our spine clinics, this is why we offer treatment options for patients throughout Hackettstown and Newton.
What are the risk factors?
Possible risk factors for ruptured disks are injury, smoking, pregnancy, jobs with heavy lifting, repetitive lifting and twisting or operation of vehicles.
Other Names for Sciatica
Bulging disk, ruptured disk, pinched nerve, herniated nucleus pulposus, disk herniation, disk protrusion, disk extrusion or disk sequestration, recurrent disk herniation
How is Sciatica Diagnosed?
MRI scan is the best test to see a herniated disk compressing a nerve. CT myelogram (contrast dye injected into the spinal canal) is usually reserved to patients who cannot have an MRI. EMG (electromyelography) can help confirm nerve irritation and injury.
Spinal injections may be used to determine if the disk is causing pain, a process called pain mapping.
How do you treat Sciatica?
Patients who fail conservative treatment may benefit from spine surgery. Traditional open spine surgery is destructive to the spine. The larger the incision the more damage to skin, muscle, ligaments and bone. This collateral tissue damage may result in more pain, back muscle weakness, instability and scar tissue leading to future difficulties.
Our endoscopic spine surgery in Hackettstown and Newton is done through a small skin incision less than 1-inch, but it is more than just a small incision. The surgery is done through a tube in between back muscles to decrease muscle damage and weakness caused by muscle retraction. Minimally invasive surgery is not the same as “microsurgery”. “Microsurgery” only refers to the use of a microscope not the size of the incision or the amount of tissue damage.
Endoscopic spine surgery is state-of–the-art minimally invasive spine surgery. Endoscopic discectomy is the removal of the disk through the endoscope. A micro video camera is inserted through a very small incision (the size of a finger nail) to the “pinched” nerve. The camera projects the images onto a video screen so the surgeon can easily see the compression. Tiny instruments are inserted through the camera to decompress the nerve relieving pain and suffering. Advantages of endoscopic discectomy are no general anesthesia, very small incision, minimal postoperative pain and shorter recovery then traditional open surgery.
Endoscopic discectomy is an excellent choice for recurrent disk herniation after traditional discectomy because it avoids most of the old scar tissue decreasing the chance of dural tears and spinal fluid leaks. Traditional discectomy is done through a midline incision. Second surgery must deal with the scar tissue from the first operation increasing risk of complications. Endoscopic surgery is done from the side of the spine instead of the rear avoiding most scar tissue and potential problems.
